1 in 7 people over 40 have COPD, I am one of them…
My name is Patricia and I have Stage 4 Chronic Obstructive Pulmonary Disease more commonly known as COPD.
I am 64 and was diagnosed with COPD at just 38 years of age. It is crazy to think that I have been living with COPD for the past 26 years…where the struggle of breathing everyday has become the story of my life.
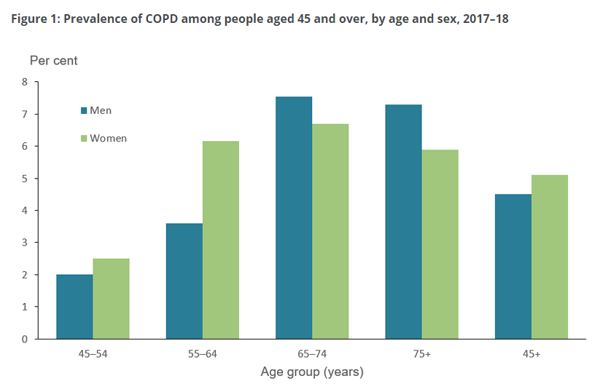
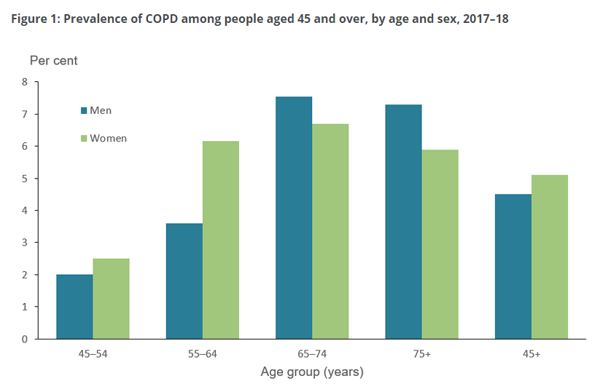
They say COPD takes years to develop and is most common for women aged 65-74 yrs. When I look at the figure below, I don’t see my diagnosis age and I haven’t read much about people having COPD in their 30s, but here I am.
In 1993, when I was first diagnosed with COPD, I found it hard to believe. I had three children aged 10, 15 and 17 and I had just been diagnosed with a serious long-term life altering disease. I was completely overwhelmed with emotion as to what my future would look like and what this meant for my children. I was thinking, how could my luck be so bad!
Back then people associated COPD with heavy smoking, in fact my lung specialist at the time thought I was lying when I said that I didn’t smoke, and still today, if I happen to see a different doctor, other than my usual lung specialist, they automatically assume I smoke/smoked. BUT to set the record straight – I have NEVER smoked a cigarette in my life and I get emotional about the stigma that comes with COPD and smoking. This prompted me to investigate other causes of COPD, how did I get it?
Looking back on my childhood, my mother had severe asthma which she was constantly struggling to manage but for me, I didn’t have asthma, but I do remember having chronic bronchitis. I remember my school teacher asking me to leave the classroom because I was disrupting the class with my coughing. They say Chronic Bronchitis can lead to COPD, could this be it? Or could it be that my father was a prisoner of war for years and when he returned, he used to smoke a lot as a way of coping with his trauma. In those days, people smoked inside the house, inside cars and you couldn’t really escape it. Was I a victim of passive smoking, which now resulted in COPD? maybe? Or could it be that I lived in Sydney where the air quality was quite polluted? we can probably rule that one out too… but who knows?

My specialist ordered an Alpha-1 antitrypsin genetic disorder test. Alpha-1 Antitrypsin Deficiency (AATD) is one of the most common genetic disorders in the world, it is often misdiagnosed. Many patients are told they have asthma, bronchitis, symptoms related to stress, emphysema caused by smoking, or simply chronic obstructive pulmonary disease of unknown cause.
The most common indicators of AATD include shortness of breath, a chronic cough, and abnormal liver test results. If you have any of these symptoms there is a simple blood test that can detect Alpha-1 Antitrypsin (AAT) levels. I was sure this was it, this was the cause, but it too came back negative. I will never actually find out what the cause of my COPD is and to be honest it doesn’t change the fact I have it.
My health and breathing had declined quite rapidly and in just four years of disease progression, I was dependent on home oxygen. My children had seen what was once, an active lively mother, become someone who was almost immobilised, someone who struggled with everyday life, someone who struggled with every breathe. I became a strong candidate for a double lung transplant and began the testing and approvals phase of the process. I felt hope, hope that I could no longer feel the pain and panic of lack of breath, hope that I could gain somewhat my life back, my health back, to only be shut down and rejected as a possible candidate due to my melanoma back in 1988. Turns out, they don’t do transplants for people who have had cancer due to risk of it coming back, or organ rejection. I was totally heart broken. My specialist at the time, pushed my case – ‘if she isn’t a candidate for a double lung, could she at least qualify for 1 lung?’ but still, it did not rule in my favour.
The only option I had was to manage the progression of the disease, continue the plethora of medications and home oxygen, attend Pulmonary Rehabilitation programs and check in regularly with my lung specialist. The realisation had set in, this was going to be my life. It wasn’t going to get any better and it was going to be an uphill battle.
In 1997, my COPD got to a point where it began to plateau, it stopped declining. At this point I had approx. 60% lung capacity, and my body had adjusted to this being my new norm. I was able to taper off the oxygen and my COPD could be managed by medication, using cortisone, oxygen and hospital visits when it flared up. I started to get more mobile and gain a bit of my independence back. I choose to stay positive and not to let my COPD define me, although some days more challenging than others, I was determined to fight the disease every day.


Most people take breathing for granted but for someone with COPD it’s a very special gift. I have experienced many ups and downs, participated in many lung trials, and apparently, I make a great test case for medical research students, having participated in practical and theory exercises in their studies, too many to count, in the hope that one day, research will find a cure.
Today, I have Stage 4 COPD (also known as end-stage) with just 23% lung capacity/function, meaning I have very little lung function and find it extremely hard to breathe in or out. Flare-ups can be life threatening and I have had at least two flare-ups this past year, resulting in long hospital stays. My lungs are putting so much pressure on my heart, that I have suffered multiple strokes and now have chronic heart disease. I need open heart surgery, but due to the lungs being so bad, once I go on life support for the operation, they are not sure my lungs or heart will start beating again. Thankfully with technology and the quality of medicine these days, and after a long approval process, I have been approved for the TAVI heart procedure which will hopefully, help me gain a few extra years of life by slowing down the progression of my COPD.
A life that despite having all these debilitating diseases and conditions, I have enjoyed. I have and continue to live each day to the fullest and not take for granted. A journey that has only been made possible through the support of my family, friends and medical professionals. I am strong and I will continue to help, support and inspire others to keep going. I have COPD, COPD does not have me!






