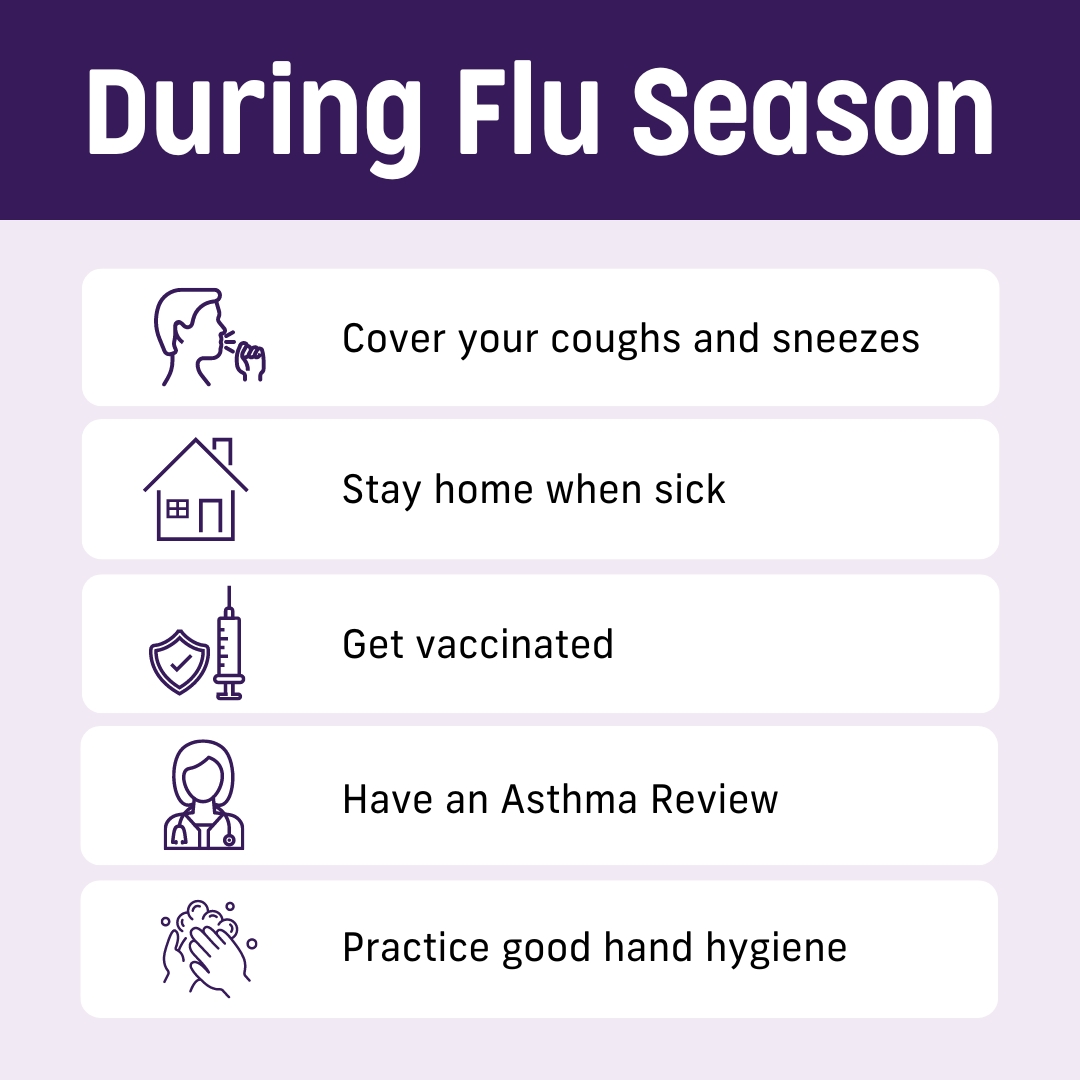
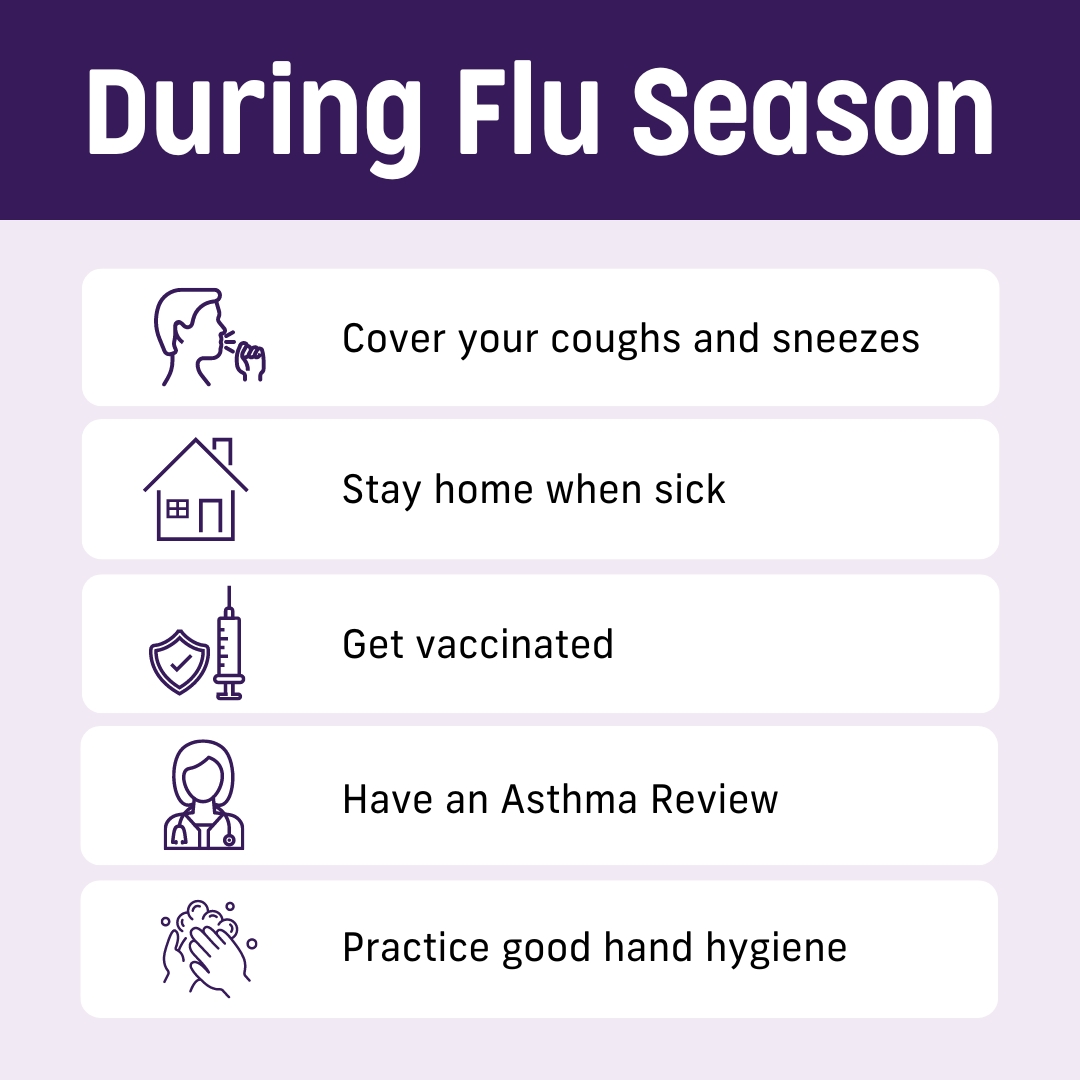
The most common trigger for asthma flare-ups in Australia is being sick with a respiratory infection like a cold or flu and other viruses. This includes asthma attacks bad enough to need a hospital visit. So, it is important to protect against respiratory infections, by practicing good hygiene (like handwashing and covering your coughs), staying home when sick, getting vaccinated and having an asthma review.
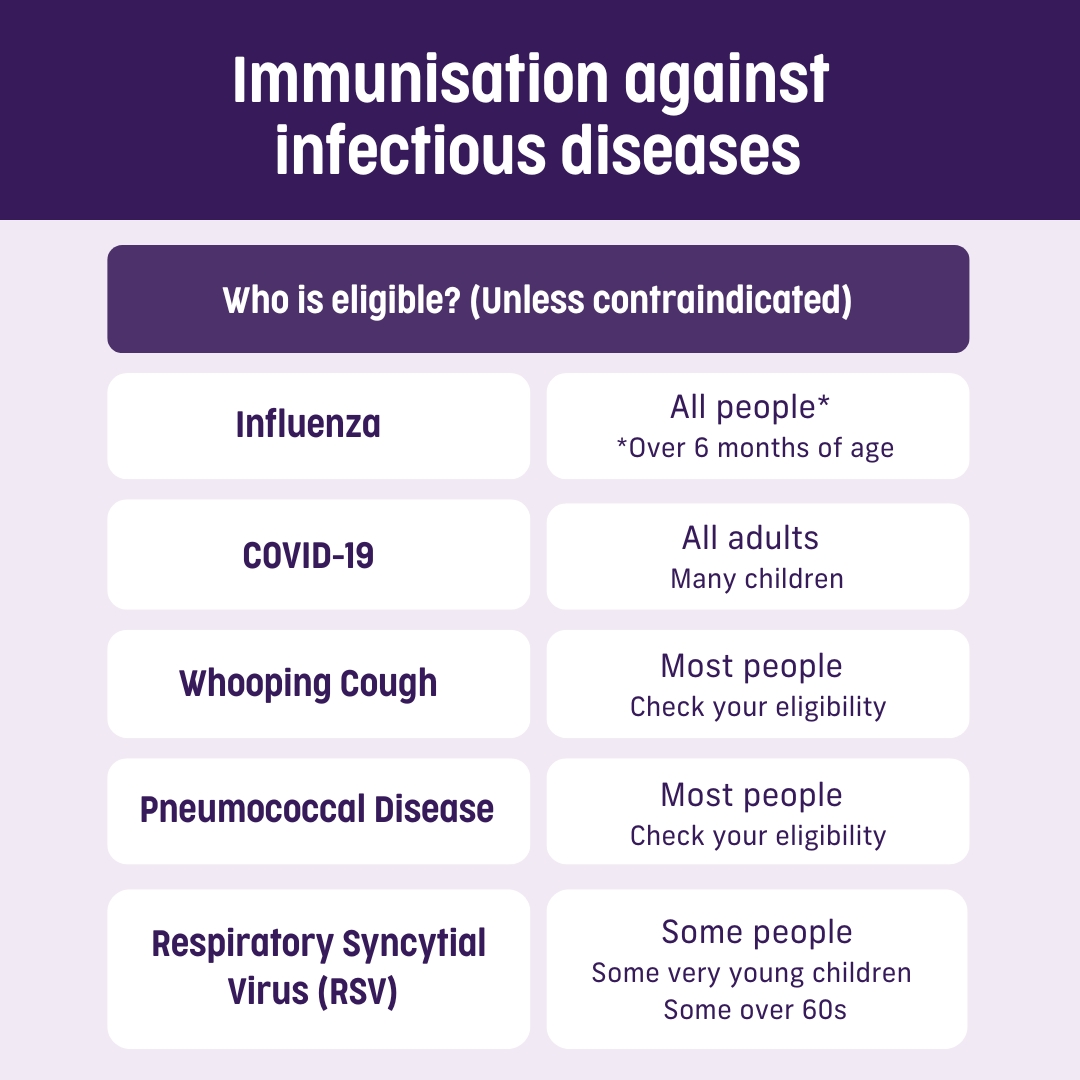
For people with asthma, immunisation is important. Immunisation is an evidence-based approach. It can prevent and protect you from respiratory infections caused by these viruses. In adults, the most common time to have your asthma triggered by a virus is over winter. That’s why the ideal time to get your flu vaccine is before winter hits.
Have you ever wondered the difference between the words: vaccine, vaccination and immunisation?
- Vaccines are the medicine used to immunise people against infectious diseases.
- Vaccination is the term used for getting a vaccine – such as when you have the injection.
- Immunisation is the process of getting the vaccine and then becoming immune once the vaccine has time to work.
There are many vaccines that help stop viruses and bacteria from making you sick. Some are free for certain people under Australia’s National Immunisation Program. Others you can choose to have, but you may have to pay out of pocket. Because respiratory infections have such a large impact on asthma, it’s worth talking to your doctor about what you can do to avoid them.
Several viruses have been linked to developing or worsening asthma. Respiratory Syncytial Virus (RSV), for example, is thought to be responsible for up to 22% of asthma risk in kids under 5, and up to 27% of asthma risk in kids aged 5-11 years! The good news is that immunisation against RSV is now available to certain groups of people.
Learn more about vaccinations for infectious diseases:
Children
Viral infections, including the flu, are the most common trigger for asthma flare-ups, including asthma attacks requiring a hospital visit.
In 2023, kids under 10 years were the most likely to get the flu, compared to older children and adults. Nearly 3 in 4 people hospitalised for flu last year were kids under 16. Although flu vaccination is free for children aged 6 months to 5 years, vaccination was particularly low in this age group.
So far this year, more children under 10 have had the flu than any other age group.
All people with asthma
Flu vaccination is recommended for all people aged 6 months and over.
Many people are eligible to receive a flu vaccine completely free, including:
• All kids aged 6 months to under 5 years
• Pregnant women (at any stage of pregnancy)
• People with certain medical conditions that increase their chance of severe influenza and its complications, including people with severe asthma
• People aged 65 and older
• Aboriginal and Torres Strait Islander people
• All Queenslanders
Check with your doctor or pharmacist to see if you are eligible and if flu vaccination is suitable for you.
An initial vaccination against COVID-19, called primary course vaccination, is recommended for:
- all adults 18 and over
- kids aged 6 months to 17 years that have a medical condition increasing their risk of severe disease from COVID-19.
The primary course can include several vaccine doses.
After having received their initial vaccination, most Australians aged 18 and over can consider receiving a booster dose every 12 months, particularly if they have a medical condition that increases their risk of severe COVID-19.
For some groups, it is highly recommended to receive a booster every 6 to 12 months. These include:
- adults aged 65 and over
- adults with severe immunocompromise
Booster doses are not usually recommended in kids. However, children aged 5 to 17 with severe immunocompromise can consider a booster dose every 12 months.
The conditions that increase the risk of severe COVID-19 include immunocompromising conditions, cardiac disease, respiratory disease including severe asthma, neurological conditions, metabolic conditions, kidney or liver disease and obesity. If your condition is not listed, your doctor may still advise you to receive a booster.
Check with your doctor if primary or booster COVID-19 vaccination is suitable for you.
Young Children
Whooping cough (or pertussis) is a very contagious respiratory infection that is usually mild in teenagers and adults but can be life-threatening for babies. Free whooping cough vaccination is usually given in childhood with several doses between the ages of 2 months and 13 years of age, but protection fades over time.
Pregnant women
If you are pregnant, you can receive a free whooping cough booster vaccine for each pregnancy, and it is usually recommended (although not free) that other people living with or caring for the infant also receive a booster dose to protect the infant.
People working with young children
Healthcare workers and other people working with young children (early childhood educators and carers) are recommended to get a booster dose every 10 years.
Adults with asthma
Although Whooping Cough is generally not severe in adults, it can be associated with worse symptoms and severe disease in people with asthma and can worsen asthma symptoms.
Whooping cough vaccination is available for any adult who wants to reduce their likelihood of becoming ill with whooping cough – however you will need to pay. Often, they are given in a vaccine which also contains a tetanus booster.
Adults aged 65 years and over are recommended to receive a combination whooping cough vaccine if they have not had one in the past 10 years. This is because whooping cough has greater risks for older people and immunity wanes over time.
Check with your doctor if you are eligible and if whooping cough vaccination is suitable for you.
Pneumococcal disease is caused by a bacteria, Streptococcus pneumoniae, which can lead to severe invasive disease like meningitis, pneumonia and bacteraemia. Pneumococcal infection can also contribute to an asthma flare-up. People with obstructive airways disease, including asthma, have a higher risk of invasive pneumococcal disease.
Young children
Pneumococcal vaccines are part of the childhood immunisation program, up to 12 months of age (free).
Children and adults with asthma
People of all ages over 12 months with a medical risk for pneumococcal disease, including severe asthma (requiring frequent hospital visits or the use of multiple medications), are recommended to receive pneumococcal vaccination (at cost for severe asthma).
Aboriginal and Torres Strait Islander people
Some children over 12 months and adults aged 50 and over can receive pneumococcal vaccination (free).
Adults 70 years and over
All adults aged 70 and over are recommended to receive a dose of pneumococcal vaccine (free).
Check with your doctor if you are eligible and if pneumococcal vaccination is suitable for you.
Young Children
RSV is the leading cause of hospitalisation due to lower respiratory tract infection and bronchiolitis in infants aged under 6 months. Most hospitalisations occur in children that are otherwise healthy.
Severe respiratory viral infections during infancy including RSV are a risk factor associated with childhood asthma.
Several immunisation products are available to help protect young children. This includes antibodies against RSV that can be given to both infants and young children, although current availability depends on the state you live in. Check with your doctor if your child is eligible and is likely to benefit from RSV antibodies. Pregnant persons may also receive an RSV vaccine during pregnancy to help protect their infant after they are born.
Pregnancy
When a pregnant person receives the RSV vaccine, antibodies against the virus are transferred through the placenta to the baby. This helps protect the baby during the first 6 months after birth when they are most likely to be very ill from RSV if they catch the virus.
A maternal RSV vaccine is free under the National Immunisation Program for people at 28–36 weeks of pregnancy (prior to 37 weeks). Check with your doctor if you are eligible for RSV vaccination during pregnancy and if it is likely to benefit your baby.
Over 60s
Although RSV in adults is usually mild, people may develop a lung infection or pneumonia. Older people are particularly at risk, with people 50 to 65 years of age having a higher chance of going to hospital due to RSV. People with a heart condition, a lung condition such as asthma, or a weak immune system, are also more likely to need hospitalisation. Your asthma can also worsen if you have an RSV infection.
For people aged 60 and over, RSV vaccination is currently available via private purchase. The National Centre for Immunisation Research and Surveillance (NCIRS) recommends RSV vaccination for all people aged 75 and over, people aged 60-74 with a medical condition increasing their risk of serious disease (including severe asthma), and First Nations people aged 60 and over. Anyone aged 60 and over can consider RSV vaccination. Check with your doctor if you are eligible and if RSV vaccination may be suitable for you.
To find out if you are eligible for a certain vaccine, check out these resources:
Watch our video that shares real life stories of our Asthma Champions – people like you – on the benefits of vaccines as part of your asthma management plan.
This video was developed independently by Asthma Australia, with support via an unrestricted grant from Sanofi

Have questions? Chat to your doctor or call one of our Asthma Educators on 1800 ASTHMA (1800 278 462). You can also book a call for a time that suits you below.
Book a call with an asthma educator
This page was developed independently by Asthma Australia, and made possible by unrestricted grants from GSK, Sanofi, AstraZeneca and Chiesi, who are not involved in content development.





 1800 278 462
1800 278 462



