Asthma, COVID-19 & Telehealth: The Doctor is Calling
It can be hard to communicate about certain health issues by phone or video feed. Asthma is different for everyone, and it can be daunting to try and communicate over the phone when you are experiencing asthma symptoms. But given the challenges of COVID-19, we’re helping you gain better outcomes from telehealth for asthma.
In this article, we look at ways to improve your experience with asthma-related telehealth appointments. Telehealth is not ideal for many people when compared to a normal doctor’s appointment. But it is far better than avoiding the doctor and letting your asthma worsen. Be proactive. Asthma prevention has never been more important. Surveys show that close to half of people with asthma have delayed a doctor’s appointment because of issues related to COVID-19 and everyone can take steps to manage and prevent flare-ups.
So, how can we make sure we are getting the most out of our telehealth appointments for asthma?
Overcoming Telehealth Concerns
Telehealth can be incredibly useful as a supplement to normal medical care. In remote Australia, telehealth has been used to overcome issues like distance and accessibility for many years. For others, telehealth is new.
You might miss the tangibility and compassion of the human touch or dislike your doctor’s inability to ‘hear your chest’. If you aren’t sure what you need to tell your doctor on the phone, let them know. Together, you can find the best ways to include telehealth as part of your toolkit to manage your asthma.
You might not know what to expect during your first telehealth appointment. Often, your GP will simply call you for the appointment on your telephone, but you can double check with the receptionist.
If telehealth isn’t your preference, explain your concerns to your doctor. Let them know you’d like to focus on more regular check-ups in person, and you want to get in control of your asthma before any symptoms flare-up over spring. Instead of delaying your visit with your doctor because of COVID-19, it’s much better to use telehealth to keep the lines of communication open, so when you are present in person, it’s a much better experience.
This Spring: Prevention is Key
Spring brings a whole host of new triggers, like pollen, hay fever and thunderstorm asthma. Our message this year is to ‘breathe your best’. It is important to think about asthma prevention, and the ways telehealth fits in with your overall asthma plan.
If spring is a time that your asthma usually flares-up, now is the time to organize an Asthma Review with your doctor – before the flare-up occurs. Make sure you are on top of your prescriptions and your medications are stocked. Remember though, that telehealth is always available if you need it.
We look at overcoming some of the common telehealth barriers below, and the ways we can monitor and prevent asthma at home this spring.
#1 – Talk to your doctor and their team
The first step to improving the ways we access telehealth is to plan our conversations with your doctor.
- Be sure to record your symptoms, such as breathing difficulty or coughing, and communicate these issues with your doctor.
- Let your doctor know how many times you have needed your reliever, and if it is giving you relief.
- Check your temperature. Knowing if you have a fever or not will help your doctor triage if you need to be seen in person and assess if it is safe for you to be seen by them.
Your doctor’s surgery will have COVID-19 procedures in place, but these might vary depending on the level of lockdown in your area, or how severe your symptoms are. Ask the receptionist what their current practice policy is with your current symptoms.
- Many medical clinics and hospitals have implemented new measures to help people experiencing COVID-19 like symptoms to access treatment in-person. These include areas where you can have your respiratory issues assessed even if you are already coughing or experiencing breathing difficulty.
- The receptionist may organise a telehealth appointment for you as a first step. Then the doctor will assess and triage if they need to see you in person and invite you in if they can do so.
- If your practice requires a negative COVID-19 test before any face-to-face appointments keep this in mind. Remember that if you have covid-like symptoms, no matter how mild, or if you think they are asthma, get tested straight away. This way you will have your result and be allowed to see your doctor as soon as possible.
- If they can’t safely see you, your GP’s receptionist will most likely know other places you can go to in your local area if you have covid-like symptoms and need to be seen in person. Ask them what they recommend you do.
#2 – Keep an Asthma Diary
An asthma diary lets you keep track of your asthma symptoms. Each day, you record important asthma information. This includes any asthma triggers you experience, the medication you take, and any symptoms you have.
These notes can be made in many ways. While some people prefer a paper diary, many people now find their mobile devices to be perfect for keeping records of their asthma. Apps are also available that can help you – such as Asthma Buddy.
Asthma diaries can also include things like asthma control scores and peak flow measurements, and we include more information on these below.
#3 – Take an Asthma Control Test
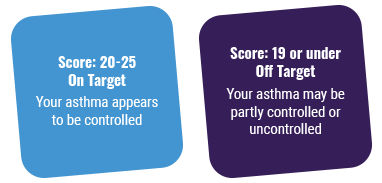
An Asthma Control Test assesses the levels of your asthma by asking a series of simple questions. The test provides an asthma score which helps you and your doctor decide if your asthma is controlled or if there is room for better management.
One of the best things about the control test is that you can do a new test periodically to see if your asthma is staying under control. If you haven’t taken an asthma control test recently, or your symptoms change, then a new control score can help you better understand your asthma. The results of an asthma control test can be given to your doctor who can use this information to better help you in the season ahead.
#4 – Peak Flow Testing

Peak flow testing measures the amount of air that is able to flow out of your lungs. Over time, these readings can be used to form a peak flow graph. These graphs help visualize the way your lung function changes each day, which can help you and your doctor to assess whether your asthma is improving.
You can talk to your doctor if you think that peak flow testing will help you. It is important that you approach these monitoring techniques with the guidance of your doctor, and you can read more about peak flow and spirometry testing here.





 1800 278 462
1800 278 462



