As lovely as spring sounds, it can be a difficult time for people with asthma. Not only are there a host of new triggers during the season, such as pollen and hay fever, but lately we have also had the return of COVID-19 and lockdowns.
We know from our survey data and the discussions we have with people with asthma, that many of us are finding our normal health appointments harder to access – particularly, if we are experiencing symptoms such as difficulty breathing, runny noses or coughing that cross over with the symptoms for COVID-19.
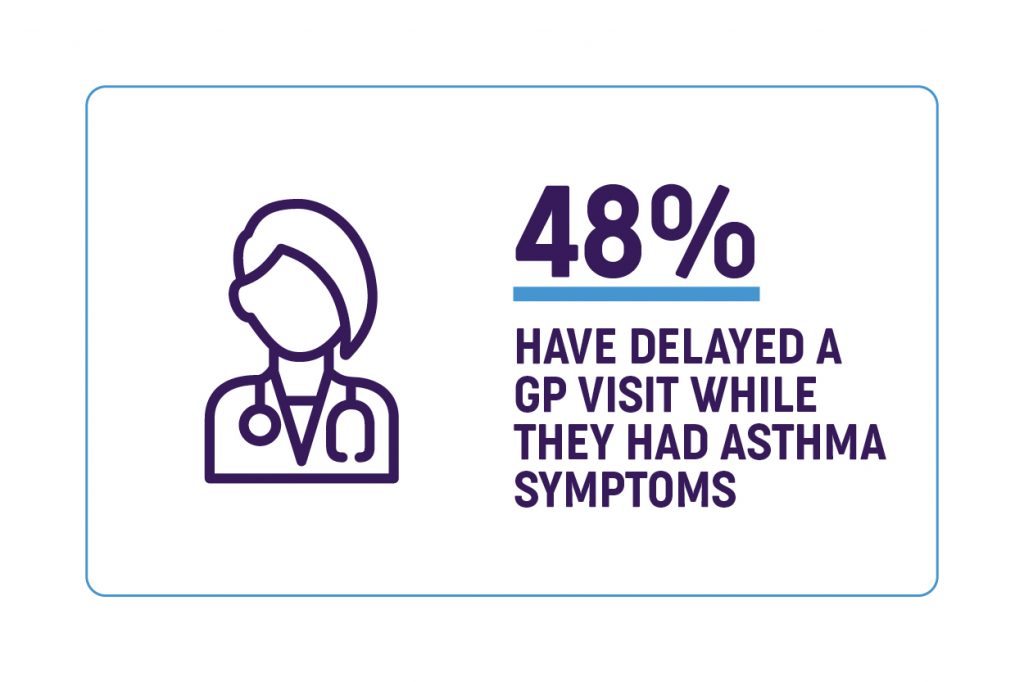
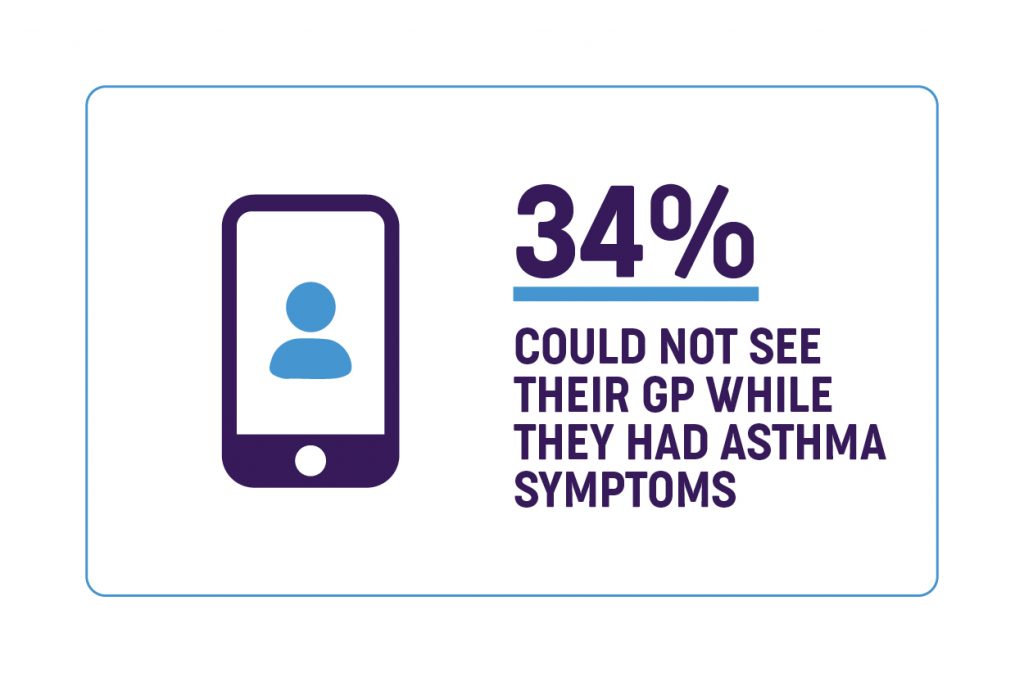
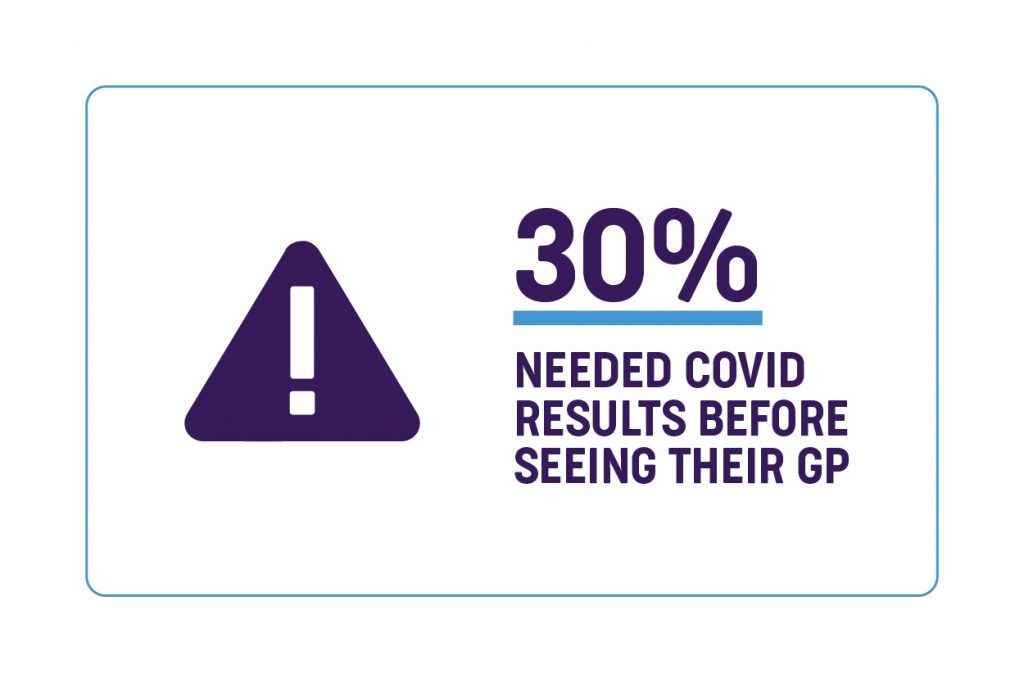
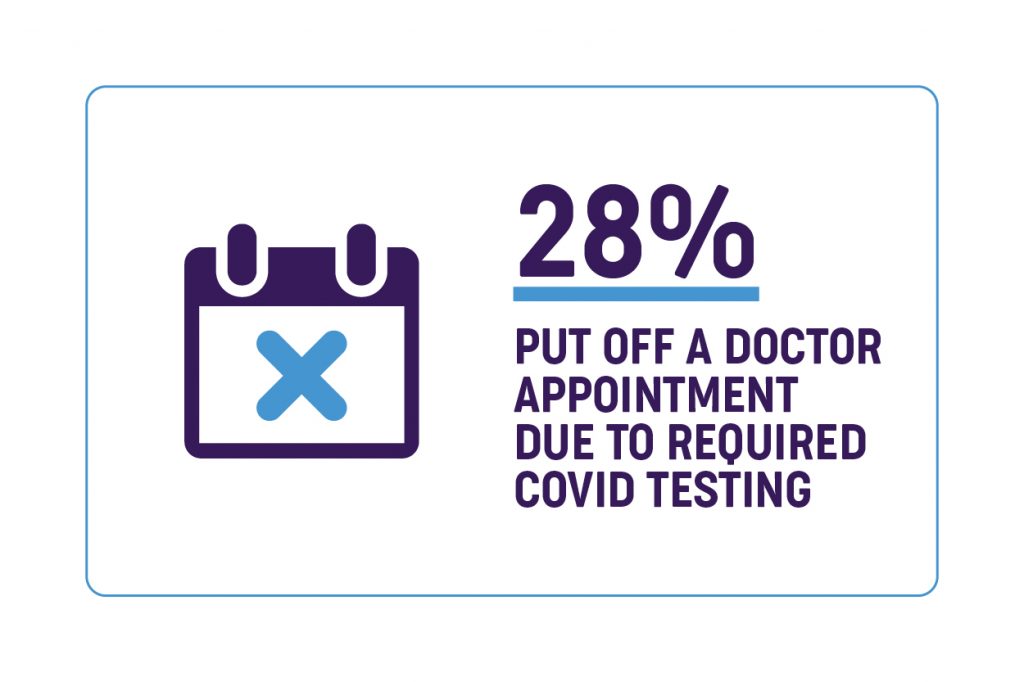
These stats are providing us with insight into the situations many people are facing, and we are actively looking to talk to people with asthma that are experiencing these issues. You can contact our asthma educators here or read more about becoming an asthma champion.
We have put together the following tips to help you access the healthcare you need this spring, and help you stay healthy and in control of your asthma and hay fever. We have had many people voice their concerns to us, and we have put together these tips to help – from taking a proactive approach to your spring asthma and allergy plan to engaging your health team using telehealth.
- Be proactive
- Use Telehealth
- Be upfront
- Don’t wait
- Call a helpline
Together, we can work towards lessening the impacts of COVID-19 and making sure that we are well prepared this spring.
5 top tips for seeing your GP during Spring and COVID-19 restrictions
Be proactive
Talk to your doctor and have a plan ready for the steps to take if your asthma worsens. This should be written out on an Asthma Action Plan for you to keep and follow at home. An Asthma Action Plan should be more detailed than your Asthma First Aid directions. Research shows that most asthma flare-ups can be self-managed at home if you have an Asthma Action Plan to follow. Read more about Asthma Action Plans here.
To keep or reach a level of good asthma control it’s important to take your preventer every day, even when you are well. This will help prevent your asthma worsening or slowly deteriorating to a point you get symptoms. Preventers take a few weeks to work fully, so please stick with it. If you don’t have a preventer yet, ask your doctor if you should be prescribed one.
Hay fever can make your asthma worse, so it’s important to keep in control. Ask your doctor or pharmacist if taking a daily steroid nasal spray would be right for you. These can help prevent and reduce hay fever symptoms.
Do you have enough of your normal medications at home? We recommend always keeping a 30-day supply of your medication available, to avoid running out. If your doctor includes any extra medications as part of your Asthma Action Plan, make sure you have those prescriptions ready to go too.
Take note of whether your local chemist has an online ordering service for prescriptions and over-the-counter hay fever medications. Setting up an account in advance might relieve some stress later if you become unwell, you experience a COVID-19 lockdown and are at high risk, or you need to quarantine.
Use Telehealth
Telehealth services with GPs (General Practitioners) have been expanded during the pandemic. Telehealth appointments mean you can speak with your doctor over the phone, or even via video chat. Depending on the current public health rules where you are, telehealth access may even be extended to new patients if you have trouble getting a telehealth appointment with your normal doctor. Read more about bulk billed telehealth appointments here.
During your telehealth appointment it will be useful to your doctor if you are prepared to tell them:
- the symptoms you or your child are having
- how often the symptoms occur
- how long reliever medication is lasting
- what your normal medications and other conditions are (especially if you are seeing a new doctor)
If your doctor believes it is important for you or your child to be seen in person, they will tell you what steps to take.
Some GPs will request that you show a negative COVID-19 test before having a face-to-face appointment. You can still request a telehealth appointment with your GP before your test or while you are waiting for your test results. This will allow you to get advice and prescriptions sorted without delay.
Be upfront

We don’t recommend denying or downplaying your symptoms to health service staff in order to see your GP face to face. The symptoms of COVID-19 are similar to asthma, and it may be impossible to distinguish them from each other. Health services must put safety first when faced with a situation where a patient’s symptoms may be caused by COVID-19.
Many GPs will still see you or your child with fever, cough, sore throat, or other COVID-like symptoms, but will conduct a risk assessment and maybe implement special protocols to keep themselves and other patients safe.
These might include:
- Asking you to call on arrival and wait outside or in your car rather than in the waiting room.
- Asking you to wear a facemask while inside the clinic (even if a mask mandate is not in effect). If you have trouble wearing a mask you can be prepared by having your preferred type of mask with you, and keep in mind it will be for a very short period. See our tips on easing into wearing a facemask here. If you can’t tolerate a facemask at all, you could politely request to wait outside, and be extra careful to maintain 1.5metres of physical distance between yourself and others.
- Seeing you in a particular room of the clinic which has appropriate ventilation and is cleaned after your visit.
- The doctor or nurse may wear extra personal protective equipment like gowns, facemasks, or face shields.
Don’t Wait.
As one of our survey respondents put it; “Asthma doesn’t wait for COVID-19”. If you are experiencing severe asthma symptoms, or don’t have an Asthma Action Plan to follow as your asthma is worsening, DON’T WAIT.
Call your regular GP clinic to see if they will see you with your current symptoms. If they can’t, ask them what they suggest you do – for example, it may be possible to have a telehealth consult or try a different health care service.
Check if there is a fever or respiratory clinic nearby set up to see people experiencing mild to moderate respiratory symptoms. Fever and respiratory clinics will usually also conduct a COVID-19 test when they see you.
In some cases, you may be told to present to your local emergency department for urgent care. Health workers in hospital emergency departments have been trained on how to manage any possible cases of COVID-19 and even if you are attending an emergency department for your asthma, you should follow their instructions.
If your asthma symptoms are severe or not responding to Asthma First Aid, always call triple zero (000) and ask for an ambulance.
Call a Helpline
If you cannot see your GP right away, and you are not sure whether your symptoms are bad enough to go to the hospital, you can call a 24 hour/ 7 day a week service to get health advice from a registered nurse.
National: Health direct – 1800 022 222
Victoria: NURSE-ON-CALL – 1300 60 60 24
Queensland: 13 HEALTH – 13 43 25 84
The registered nurse will help you decide the best course of action to deal with you or your child’s current symptoms.
You can call our Asthma Educators on 1800 ASTHMA (1800 278 462) if you need information about managing you or your child’s asthma, particularly during the current COVID-19 response. We are available Monday – Friday, 9am-5pm.

Flo, White Magic and echamber are campaign partners of Asthma Australia and have not been involved in the development of this webpage





 1800 278 462
1800 278 462



