Asthma Australia has been monitoring the COVID-19 situation since it began in 2020.
If you have asthma and get COVID-19:
- Try to stay calm, most people will experience only a mild disease
- Let your doctor know, especially if you have any symptoms you are concerned about.
- Early use of anti-viral medicines can make a difference. Ask your doctor if these are suitable for you.
- Follow the information on https://www.healthdirect.gov.au/managing-covid-19/what-to-do
If you have uncontrolled asthma and get COVID-19
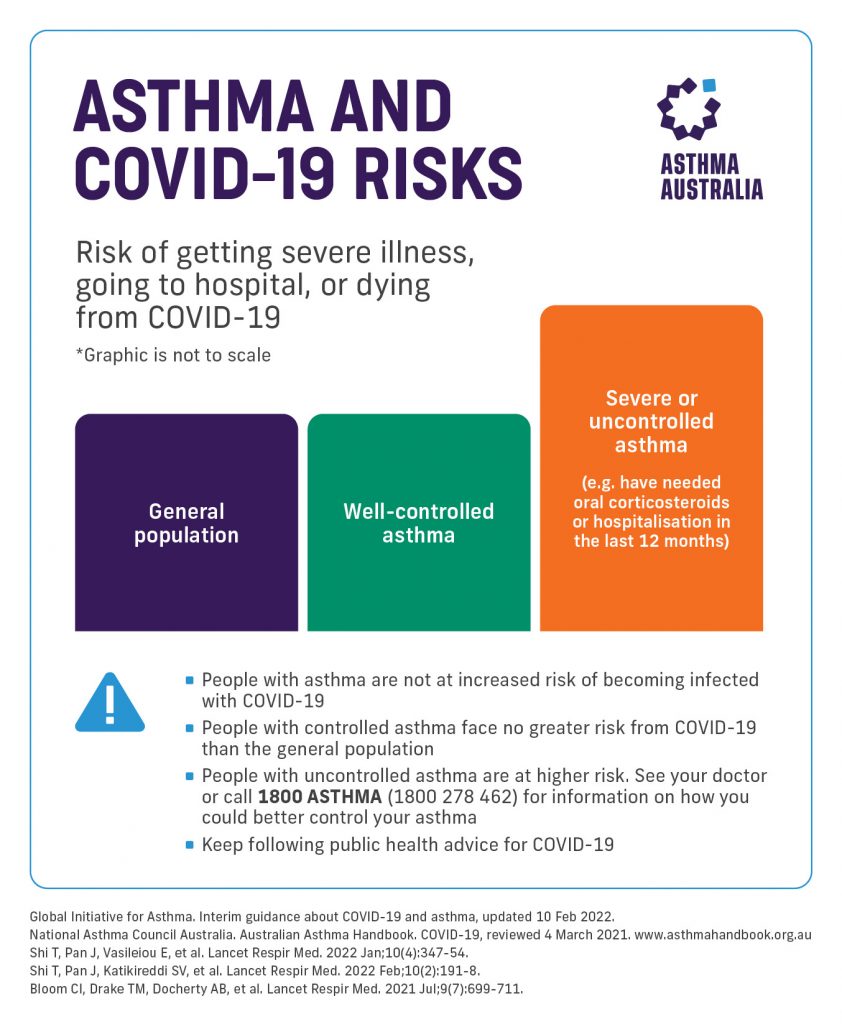
Research has found that people with uncontrolled asthma may be more likely to develop severe symptoms and be hospitalised. This includes people with asthma who:
- Have been hospitalised in the past 12 months due to an asthma flare up
- Have needed a course of oral corticosteroids for their asthma in the past 12 months (e.g. prednisone or prednisolone tablets)
If either of these apply to you, talk to your doctor about how you can get your asthma under control to lower your COVID-19 risk. For more information about asthma, you can also call us on 1800 ASTHMA (1800 278 462) or email [email protected] .
What is good asthma control?
Good asthma control means you have:
- Symptoms no more than 2 days a week
- Use your reliever no more than 2 days a week
- Aren’t limited by your asthma
- Don’t get symptoms at night or when you first wake up
To learn more about good asthma control see: https://asthma.org.au/treatment-diagnosis/live-with-asthma/talk-asthma/
Asthma and COVID-19 Risk
A lot of research has emerged since the start of the pandemic, showing that people with asthma are not at higher risk of getting COVID-19. In fact, some reports even suggest that people with asthma may generally be less likely to get COVID-19!
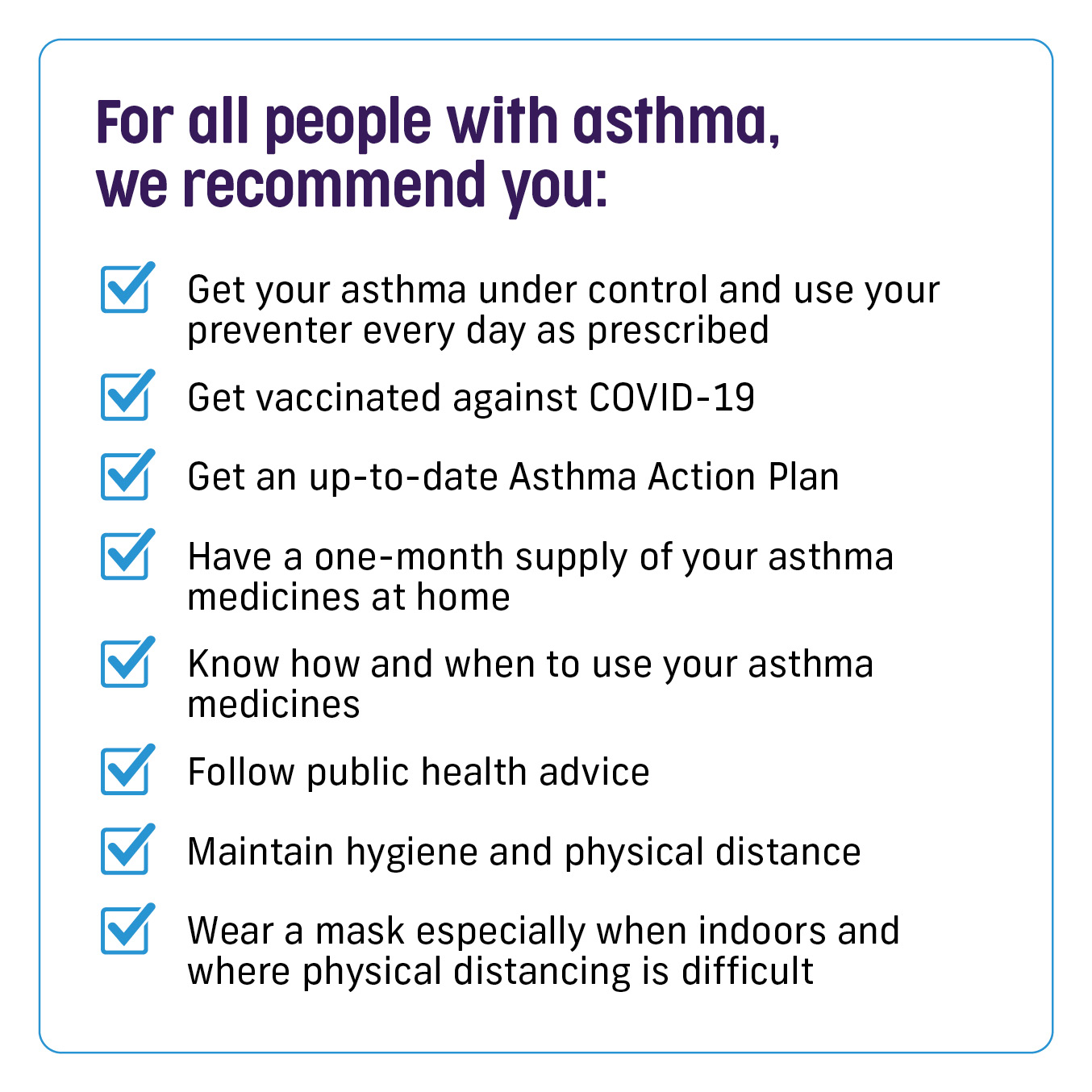
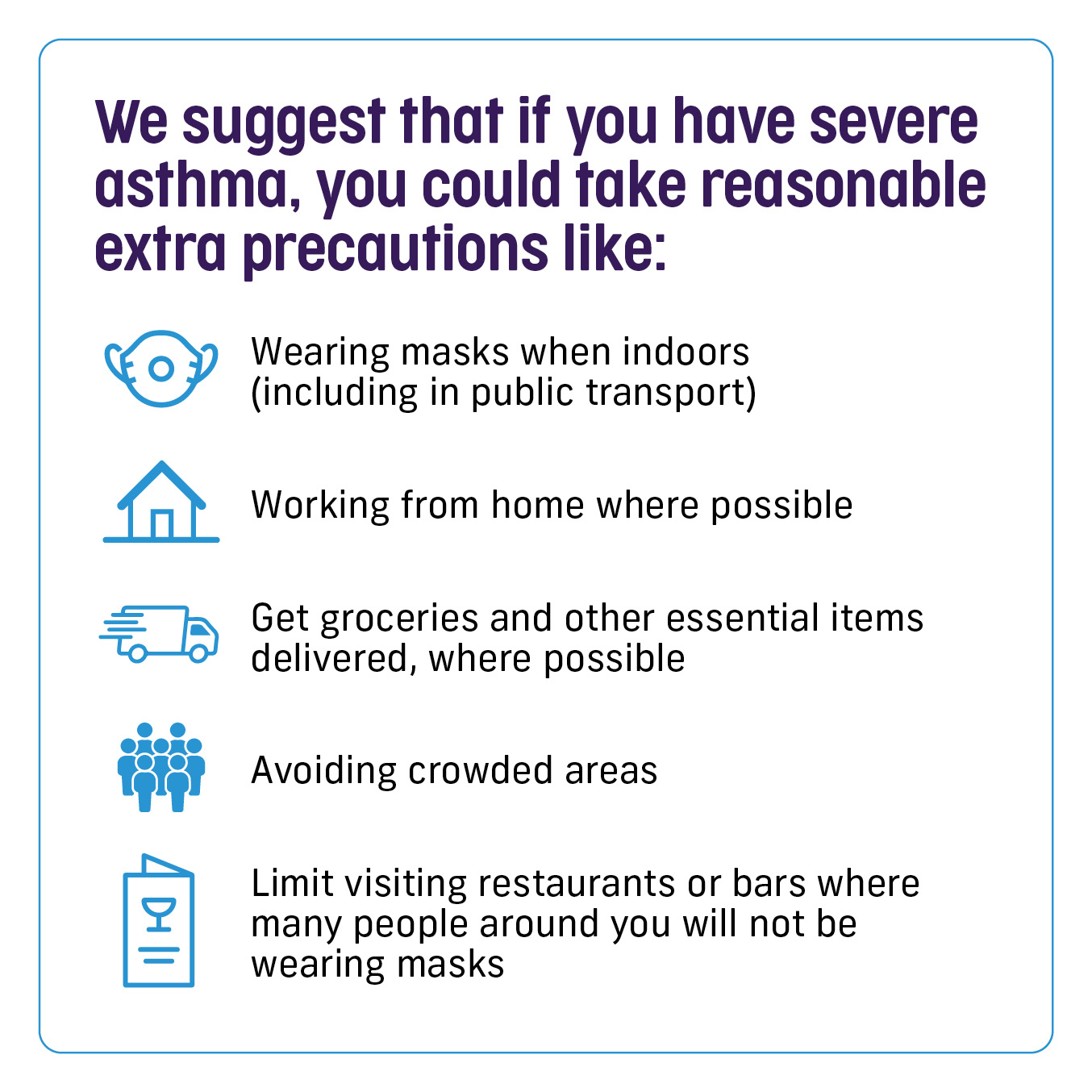
We now understand that having severe or uncontrolled asthma may be a factor that worsens COVID-19 outcomes. If you have recently been hospitalised because of your asthma or needed a course of oral steroids, you may have severe or uncontrolled asthma.
COVID-19 Symptoms
Most people with COVID-19 will only have mild symptoms. It may be hard to tell the difference between COVID-19 symptoms and your normal asthma symptoms. If you’re unsure and your asthma medicines don’t seem to be working as well as they should, talk to your doctor and get tested for COVID-19.
During the first week of having COVID-19, symptoms are often quite mild, such as sore throat, cough and fever.
Some people may have the virus and never show symptoms at all. The virus is most easily passed on to others during the first week of being sick.
During days 4–9 of feeling sick, symptoms can worsen, with more breathlessness and cough. Stomach symptoms (e.g. pain, diarrhoea) occur in around 10% of patients.
While most people recover from COVID-19 within four weeks, some people may need longer. When people still have symptoms of COVID-19 after 4 weeks, this is often called ‘Long COVID’. Some people also use the term ‘post-COVID-19 condition/syndrome’ to describe Long COVID that lasts more than 12 weeks without being explained by another condition.
Because Long COVID and asthma can be difficult to tell apart, talk to your doctor if your asthma symptoms are not getting better or you’re still not feeling well. For more information visit our Long COVID page.
COVID-19 TESTING
There are several ways to check whether your symptoms are from COVID-19.
Rapid Antigen Tests (RATs) are the most common method for home use. The Therapeutic Goods Administration (TGA) has published a list of COVID-19 rapid antigen self-tests that are approved in Australia.
You can now test at home for COVID-19 and other common respiratory viruses in the one test. These combination RATs test for COVID-19 and Influenza A/B (Flu), or COVID-19, Influenza A/B and Respiratory Syncytial Virus (RSV). These respiratory infections often have similar symptoms and can worsen asthma. For more information visit our Colds, Flu and Viruses page, and talk to your doctor or pharmacist.
There is also a page providing information on the sensitivity of the home test kits and which COVID-19 variants are found.
If using saliva for a COVID-19 self-test, it is recommended not to eat, drink, smoke, brush your teeth, or chew gum for 10-30 minutes (refer to the instructions provided with your test kit for the recommended timing) before collecting your saliva. This may produce an incorrect result.
Contact your local COVID-19 health department if you would like any further support on COVID testing.
COVID-19 VACCINES AND ASTHMA
Being vaccinated against COVID-19 is the best way to reduce your risk of severe disease. Asthma Australia strongly supports the COVID-19 vaccination program.
All Australians aged 5 years or older are eligible to have a free COVID-19 vaccine. If you or your child have asthma, you should feel confident to get a COVID-19 vaccine.
Children from 6 months to under 5 who are at increased risk of severe COVID-19 symptoms (those who have a weak immune system, have a disability, as well as those who have complex and/or multiple health conditions) are recommended for COVID-19 vaccination. Please discuss this with your doctor.
The initial COVID-19 vaccination, also called ‘primary course’, includes 2 to 3 consecutive doses of the vaccine depending on age and situation. After the primary course, you may be eligible for additional doses called ‘boosters’. More info here.
COVID-19 Vaccine Boosters:
Boosters help to maintain your protection against COVID-19.
You are eligible for a COVID-19 booster dose if it has been 6 months or longer since your last vaccine dose or COVID-19 infection and you:
- Are 18 years and older. A booster dose is particularly recommended for people that are at higher risk of getting severely ill, including people that:
- Are 65 years and over OR
- Have medical conditions, disability or complex health needs
- Are 5 to 17 years old and have a health condition increasing their risk of severe COVID-19 illness
People at higher risk of severe illness should have their next booster as soon as possible.
All vaccines approved in Australia provide strong protection against severe illness however it is recommended to receive Omicron-bivalent vaccines for boosters. Booster doses increase your protection against:
- Getting sick with the virus that causes COVID-19
- Severe disease
- Dying from COVID-19.
All booster doses are free if you are eligible. Check with your vaccine provider.
If you have any questions, speak to your doctor or call us on 1800 ASTHMA (1800 278 462).
Breathe Better Under Your Facemask
Over the past two years, face masks have become a staple of everyday life – serving as a welcome safety measure for many and even as a fashion item for a few. If you’re struggling to breathe with a face mask, you’re not alone – here are some breathing techniques to help.
Face Mask/Coverings- Tips to Ease Into Wearing One
Never before have Australians been faced with mandates on face masks/coverings and it can be both confronting and confusing for people with respiratory conditions. It’s deemed an effective strategy against community transmission of COVID-19, but we understand it’s not that easy for some. Here are a few tips to help
Cough Cough, It's my Asthma Not COVID-19
People with asthma can have a dry cough and having asthma often comes hand in hand with hay fever, which causes sneezing and a runny nose, similar symptoms to a cold. But how do you deal with having these symptoms amid a Coronavirus pandemic? If this is you or your child, here is how you can help support them in public.
Our Top Tips for Seeing Your GP During Spring and COVID-19 Restrictions
As lovely as spring sounds, it can be a difficult time for people with asthma. Many of us are finding our normal health appointments harder to access – particularly, if we are experiencing symptoms such as difficulty breathing, runny noses or coughing that cross over with the symptoms for COVID-19.
Asthma, COVID-19 & Telehealth: The Doctor is Calling
It can be hard to communicate about certain health issues by phone or video feed. Asthma is different for everyone, and it can be daunting to try and communicate over the phone when you are experiencing asthma symptoms. But given the challenges of COVID-19, we’re helping you gain better outcomes from telehealth for asthma.
Nebulisers During COVID-19
Health experts believe the use of a nebuliser may have spread the UK variant of the Coronavirus to others through airborne droplets as a nebuliser aerosolises virus particles.
The Asthma Cough
Asthma cough can be challenging. It can be embarrassing or awkward to have an ongoing cough, especially amid increased anxiety over health during COVID-19 times. Here is what you need to know about asthma cough.
Mental Health and COVID-19
Everyone reacts differently to stressful situations. During COVID-19, we’ve found ourselves physically distancing from friends and family, self-isolating for our own safety, out of work due to lockdown restrictions, and keeping our children home to partake in remote learning.
Still have more questions about asthma and COVID-19?
Speak to an Asthma Educator today by calling 1800 ASTHMA | 1800 278 462
They operate 9:00 am – 5:00 pm Monday to Friday, alternatively, you can book a call here and we’ll have someone call you back as soon as possible during business hours.





 1800 278 462
1800 278 462