CORONAVIRUS (COVID-19) AND PEOPLE WITH ASTHMA
For latest Coronavirus and Asthma information please visit our COVID-19 page.
UPDATED 16/03/2020
You might have heard that Coronavirus affects the respiratory system and you might have questions around what this means for you, or your child if they have asthma?
What is Coronavirus and COVID-19
Coronaviruses are from a family of viruses that make people sick, such as common colds and other upper respiratory tract infections.
The World Health Organisation is referring to this new Coronavirus as COVID-19, which originated in Hubei Province, China in late 2019.
Latest information and resources
Coronavirus (COVID-19) outbreak is a developing situation around the world. The most up-to-date information for Australians is on the Australian Government website here. You can also access helpful resources such as fact sheets and FAQs here. If you have any concerns, call the Australian Government Coronavirus Health Information Line on 1800 020 080.
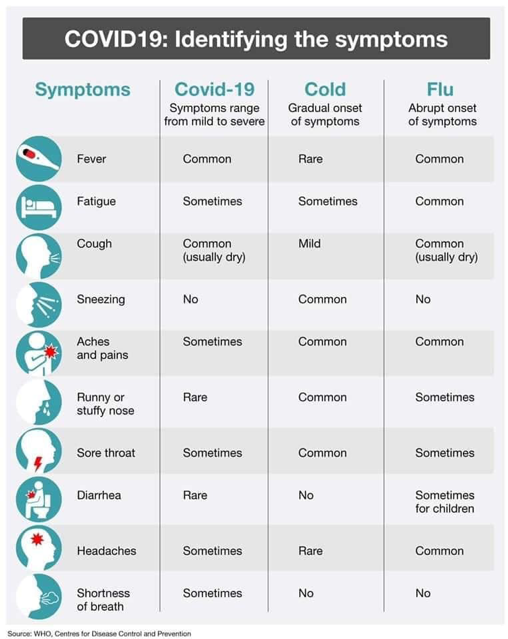
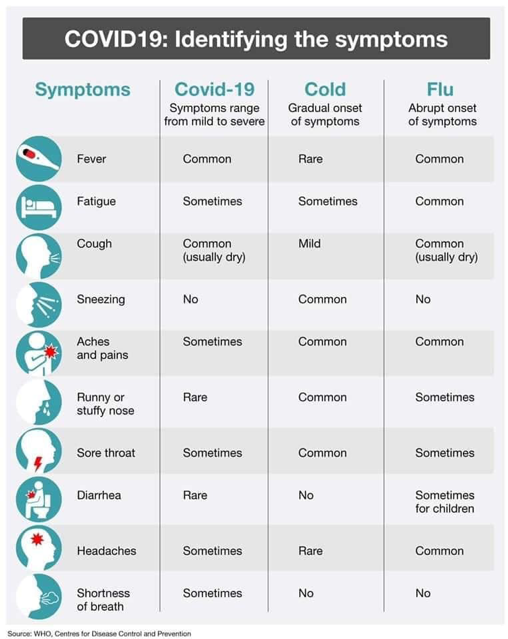
Symptoms
According to the World Health Organisation, “common signs of infection include respiratory symptoms, fever, cough, shortness of breath and breathing difficulties. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure and even death.” Most infections are only transmitted by people when they have symptoms.
COVID-19 has been declared by the World Health Organisation as a pandemic.
Prevention
To help slow the spread in Australia the government has advised effective from Monday 16 March, any organised, non-essential gatherings of 500 people or more should not proceed, anyone entering the country will be required to self-isolate for 14 days from midnight 15th March and that schools should refrain from activities such as school assemblies and excursions and be implementing social distancing strategies. View more specifics here.
In Australia, the people most at risk of getting the virus are those who have:
- recently been to a high-risk country, view here.
- been in close contact with someone who is a confirmed case of Coronavirus
View ‘When to be tested’ video from the Chief Medical Officer here. I can find further information including resources in another language at health.gov.au
Who is at highest risk for getting very sick from COVID-19?
Some people who are infected may not get sick at all, some will get mild symptoms from which they will recover easily, and others may become very ill, very quickly.
From previous knowledge with other Coronaviruses, the people most at risk of serious infection are:
- people with compromised immune systems (e.g. cancer)
- people with diagnosed chronic medical conditions
- elderly people
- Aboriginal and Torres Strait Islander people
- very young children and babies*
*At this stage the risk to children and babies, and the role children play in the transmission of COVID-19, is not clear. However, there has so far been a low rate of confirmed COVID-19 cases among children, relative to the broader population.
People with asthma
There is no specific data as yet to determine if asthmatics are at a higher risk of contracting the virus. However, a common trigger for worsening asthma symptoms for asthma flare-ups or asthma attacks are respiratory infections such as colds and viruses. COVID-19 is a respiratory virus.
From the information gathered so far, people with a chronic medical condition like asthma may be at more risk of a serious Coronavirus infection compared to those without chronic medical conditions. The primary point is to do what you can, as usual, to avoid cold and flu; pay close attention to personal hygiene, wash hands regularly, avoid close contact with people with symptoms and obtain a flu vaccination as soon as possible.
When it comes to managing your asthma, here is a checklist you can follow;
- Ensure you are on a preventer, taking it as prescribed and have a written Asthma Action Plan. You can go back to your GP at any time if you think your medication needs adjusting or if you don’t have a written Asthma Action Plan.
- Ensure you have access to a reliever puffer, always
- Ensure you can identify asthma symptoms and can treat them properly; do you know asthma first aid?
- Ensure you understand what your asthma triggers are and how to manage these (it will help having a written Asthma Action Plan).
- If you have allergies such as hay fever, ensure you are treating them
- Tell your family and friends you have asthma and make sure they also know asthma first aid and your triggers
You can ask us questions by emailing us or by calling us on 1800 ASTHMA
Planning ahead
Recommendations from the Australian Government refer to “social distancing”. Social distancing is reducing your non-essential contact with others. This would include avoid crowded spaces. You can learn more about social distancing here.
In essence, it means:
- Staying home when unwell
- Avoiding large public gatherings if not essential
- Keeping 1.5 metres from other people when possible
- Avoiding physical contact where possible (avoiding kissing, handshaking, hugging).
Making sure you have access to your current medications and having an emergency kit prepared is good practice for any emergency situation.
Asthma medication
As of 6 March 2020, and recent update on 13 March, the Therapeutic Goods Administration (TGA) has not received any notifications of medicine shortages in Australia that are a direct result of COVID-19. Therefore, while it may be appropriate for individuals to ensure that they have at least 30 days supply of prescription medicines in the unlikely event they are quarantined, any stockpiling of medicines is unnecessary. Read media release here.
As well as treating your asthma, there are other easy steps everyone can take to lower risk of a viral infection. You can view these steps via video from the World Health Organisation (WHO) below.
How is this Coronavirus spread?
The Coronavirus is most likely to spread from person-to-person by:
- direct close contact with a person while they are infectious
- close contact with a person who has been confirmed infected who coughs or sneezes, or
It can also spread from contact with infected surfaces or objects:
- touching objects or surfaces (such as door handles or tables) contaminated from a cough or sneeze from a person with a confirmed infection, and then touching your mouth or face so keeping up with good personal and hand hygiene is very important.
How can we help prevent the spread of COVID-19?
Practising good hand and sneeze/cough hygiene is the best defence against most viruses. You should:
- Avoid close contact with people who are sick.
- Avoid touching your eyes, nose, and mouth.
- Stay home when you are sick.
- and if unwell, avoid contact with others (stay more than 1.5 metres from people).
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash.
If you do not have a tissue, cough or sneeze into the bend of your elbow or in your upper sleeve. This reduces the risk of contamination because these body parts do not come into contact with people or objects
Clean and disinfect frequently touched objects and surfaces using a regular household cleaning spray or wipe.
Wash your hands often with soap and water.
Links to helpful prevention resources:
Should I wear a face mask?
You do not need to wear a mask if you are healthy. While the use of masks can help to prevent transmission of disease from infected patients to others, masks are not currently recommended for use by healthy members of the public for the prevention of infections like Coronavirus.
Visit Health Direct for further reading .
View previous communication from Asthma Australia
Coronavirus and asthma blog 28 Feb







